global Point Of Care
Antimicrobial resistance (AMR) poses a significant threat to global health, economies, and societies.
In July 2022, the European Commission identified antimicrobial resistance as one of the top three global health threats.1 The Lancet’s recent series on AMR underscores the human cost of this crisis. According to the series, nearly five million deaths per year are associated with drug-resistant bacteria, disproportionately impacting low- and middle-income countries.2
Health Consequences
AMR undermines our ability to treat common infections, resulting in prolonged illness, disability, and increased mortality. Without effective antimicrobials for the prevention and treatment of infections, the success of major surgeries or chemotherapies could be compromised.3
Economic and Social Impact
Antibiotic resistance is already associated with high costs.4,5,6 Most of the costs are caused by longer hospitalizations to treat the consequences of AMR.6 The costs of AMR will be‑borne most severely by future generations, impacting economic stability and increasing severe poverty as early as 2030.7,8
The Increasing Challenge of Antimicrobial Resistance
There is a concerning increase in the number of deaths associated with infections with antibiotic-resistant bacteria. Around 4.71 million deaths , were associated with bacterial AMR in 2021, and it´s estimated that 8.22 million deaths could occur in 2050.14
More than half of Klebsiella pneumoniae and Acinetobacter spp. infections in bloodstream cases show resistance to treatment.15


The Increasing Challenge of Antimicrobial Resistance
There is a concerning increase in the number of deaths associated with infections with antibiotic-resistant bacteria. Around 4.71 million deaths , were associated with bacterial AMR in 2021, and it´s estimated that 8.22 million deaths could occur in 2050.14
More than half of Klebsiella pneumoniae and Acinetobacter spp. infections in bloodstream cases show resistance to treatment.15


Combating AMR by Reducing Antibiotic Over‑Prescription in Primary Care Settings
The misuse and overuse of antibiotics is a significant contributor to rising antimicrobial resistance.9 In Europe, more than 90% of all antibiotic prescriptions for humans occur in community settings10, with acute respiratory tract infections (aRTIs) being by far the most common reason for prescribing antibiotics in primary care.11,12 A large proportion of these antibiotic prescriptions are estimated to be inappropriate as most aRTIs are caused by viral or self-limiting bacterial infections.11,12,13 Currently, in most countries treatment decisions are usually based on examining patient symptoms without diagnostic confirmation of a bacterial infection.
Navigating the Challenges of Antimicrobial Stewardship in
Clinical Practice
Antimicrobial stewardship is a critical strategy in the fight against AMR. There is consensus that antibiotic resistance development and spread can be curtailed by limiting antibiotic use, discouraging misuse, and reducing the burden of infectious disease. A well-functioning Antimicrobial Stewardship Program (ASP) is instrumental in accomplishing these goals. Importantly, it plays a critical role in broad-based, larger-scale efforts to help preserve our antibiotic resources for future generations.
One particularly valuable tool in antimicrobial stewardship is C-reactive protein (CRP) testing, to differentiate between self-limiting infections and severe infections. By using CRP testing, healthcare providers can make more informed decisions about whether antibiotics are needed.16

Get Expert Advice on Antimicrobial Stewardship from ENASPOC
The European Network for Antibiotic Stewardship at the Point-of-Care (ENASPOC) is a multi-disciplinary initiative aimed at improving antibiotic stewardship in primary care. It was established to address the urgent threat of AMR, which is exacerbated by the over-prescribing of antibiotics, particularly for respiratory tract infections (RTIs).17
ENASPOC focuses on implementing proven strategies, such as CRP point-of-care testing, to guide antibiotic prescriptions more effectively. For healthcare professionals, ENASPOC offers valuable resources and support to enhance their antibiotic stewardship efforts, including training materials, scientific evidence, and best practices to help improve patient outcomes and effectively combat AMR.
The group of ENASPOC experts published their recommendations about the use and the interpretation of CRP POC values in adults and in children presenting with RTIs and key messages for communication with patients and parents.18,19 Additionally, they published their recommendations for the implementation of CRP POCT.16
Get Expert Advice on Antimicrobial Stewardship from ENASPOC
The European Network for Antibiotic Stewardship at the Point-of-Care (ENASPOC) is a multi-disciplinary initiative aimed at improving antibiotic stewardship in primary care. It was established to address the urgent threat of AMR, which is exacerbated by the over-prescribing of antibiotics, particularly for respiratory tract infections (RTIs).17
ENASPOC focuses on implementing proven strategies, such as CRP point-of-care testing, to guide antibiotic prescriptions more effectively. For healthcare professionals, ENASPOC offers valuable resources and support to enhance their antibiotic stewardship efforts, including training materials, scientific evidence, and best practices to help improve patient outcomes and effectively combat AMR.
The group of ENASPOC experts published their recommendations about the use and the interpretation of CRP POC values in adults and in children presenting with RTIs and key messages for communication with patients and parents.18,19 Additionally, they published their recommendations for the implementation of CRP POCT.16
Get Expert Advice on Antimicrobial Stewardship from ENASPOC
The European Network for Antibiotic Stewardship at the Point-of-Care (ENASPOC) is a multi-disciplinary initiative aimed at improving antibiotic stewardship in primary care. It was established to address the urgent threat of AMR, which is exacerbated by the over-prescribing of antibiotics, particularly for respiratory tract infections (RTIs).17
ENASPOC focuses on implementing proven strategies, such as CRP point-of-care testing, to guide antibiotic prescriptions more effectively. For healthcare professionals, ENASPOC offers valuable resources and support to enhance their antibiotic stewardship efforts, including training materials, scientific evidence, and best practices to help improve patient outcomes and effectively combat AMR.
The group of ENASPOC experts published their recommendations about the use and the interpretation of CRP POC values in adults and in children presenting with RTIs and key messages for communication with patients and parents.18,19 Additionally, they published their recommendations for the implementation of CRP POCT.16
Key Strategies and Interventions
The team of international experts from the ENASPOC initiative encourages healthcare regulators and policymakers to enable the broader application of CRP POCT and complementary strategies in primary care for patients with RTIs.16
They suggest the following interventions:
- Include CRP POCT in Guidelines and AMR Reports and Action Plans: Integrating CRP testing into clinical guidelines and AMR strategies ensures its widespread adoption.
- Ensure CRP POCT is Implemented Together with Complementary Strategies: Combining CRP testing with other interventions enhances its effectiveness.
- Provide Adequate Reimbursement for CRP POCT and Complementary Strategies: Financial incentives support the adoption of CRP testing.
- Enable High-Quality and Primary Care-Friendly POCT Organization and Performance: Ensuring the quality and accessibility of CRP testing in primary care settings is essential.
- Enable Data Gathering, Sharing, and Discussion as Incentivization for Proper Behaviours: Data-driven approaches with audit and feedback encourage best practices.
- Generate Context-Specific Pilots and Evidence Where Needed: Tailored interventions based on local needs and evidence improve outcomes.
- Increase Public Awareness: Educating the public about AMR and the role of CRP testing fosters responsible antibiotic use.
- Ensure Healthcare Professionals’ Awareness and Understanding: Training and education for healthcare providers are crucial for effective implementation.
Role of CRP Testing in Reducing Antibiotic Misuse
The misuse and overprescription of antimicrobials, including antibiotics for viral and self-limiting bacterial infections, are key contributors to the escalating problem of antimicrobial resistance.
Point-of-care C-reactive protein (CRP) testing has emerged as an essential tool in combatting AMR, helping healthcare professionals to make informed decisions about antibiotic use. CRP POCT offers a quick and reliable indicator to better understand the severity of an infection and to understand if an infection is self-limiting or not. A large part of the antibiotics consumed in the community is estimated to be used inappropriately as the majority are self-limiting (viral or bacterial) infections and patients would not benefit from antibiotics.16,18,19 Most of respiratory tract infections (RTIs) are viral and therefore antibiotics have no clinical benefit and yet RTIs are one of the most common reasons for unnecessary antibiotic prescribing.11,12,13 High CRP values are helpful in identifying those patients who need antibiotic treatment.
Recently CRP POCT has been highlighted by OECD and WHO as a useful tool for Antibiotic Stewardship to tackle AMR.6,20
Benefits of Point-of-Care CRP Testing
Rapid Results
CRP POCT provides quick results, enabling timely clinical decisions. Rapid diagnostics may decrease the amount of inappropriate prescribing by shortening the time to receive a test result and guiding treatment decisions. The decrease in the amount of time to analyse a result considerably benefits disease management.21,22
Informed Clinical Decision-Making
Accurate CRP levels help healthcare providers determine the necessity of antibiotics. With quick evidence-based decisions, we can expect better patient outcomes, while supporting antibiotic stewardship programmes.
Reduced Unnecessary Antibiotic Prescriptions
As a marker of severity of an infection, CRP testing supports decisions about antibiotic prescribing for respiratory tract infections and therefore reduces the misuse of antibiotics. Studies have demonstrated that CRP is an available and proven tool and can safely and cost-effectively reduce antibiotic prescriptions in primary care.11,16,23
Supports Communication with The Patients
Patients may have the expectation to get antibiotics prescribed. To have a CRP available during the visit of a patient may support the communication with patients to convince them once antibiotics are not given additional benefit. Key messages for the communication with adult patients and with parents can be found in the publications of the ENASPOC experts.18,19
Cost-Effectiveness of CRP POCT and Communication Skills Training
Recent systematic reviews concluded that CRP point-of-care testing and communication skills training are cost-effective or cost-beneficial strategies for reducing inappropriate antimicrobial prescribing.23,24 These interventions can help mitigate the financial strain on healthcare systems by reducing unnecessary antibiotic use and associated costs.


Benefits of Point-of-Care CRP Testing
Rapid Results
CRP POCT provides quick results, enabling timely clinical decisions. Rapid diagnostics may decrease the amount of inappropriate prescribing by shortening the time to receive a test result and guiding treatment decisions. The decrease in the amount of time to analyse a result considerably benefits disease management.21,22
Informed Clinical Decision-Making
Accurate CRP levels help healthcare providers determine the necessity of antibiotics. With quick evidence-based decisions, we can expect better patient outcomes, while supporting antibiotic stewardship programmes.
Reduced Unnecessary Antibiotic Prescriptions
As a marker of severity of an infection, CRP testing supports decisions about antibiotic prescribing for respiratory tract infections and therefore reduces the misuse of antibiotics. Studies have demonstrated that CRP is an available and proven tool and can safely and cost-effectively reduce antibiotic prescriptions in primary care.11,16,23
Supports Communication with The Patients
Patients may have the expectation to get antibiotics prescribed. To have a CRP available during the visit of a patient may support the communication with patients to convince them once antibiotics are not given additional benefit. Key messages for the communication with adult patients and with parents can be found in the publications of the ENASPOC experts.18,19
Cost-Effectiveness of CRP POCT and Communication Skills Training
Recent systematic reviews concluded that CRP point-of-care testing and communication skills training are cost-effective or cost-beneficial strategies for reducing inappropriate antimicrobial prescribing.23,24 These interventions can help mitigate the financial strain on healthcare systems by reducing unnecessary antibiotic use and associated costs.


Improve the way you diagnose, monitor, and treat patients with Afinion™ 2
Abbott offers a best-in-class rapid diagnostic which enables healthcare practitioners to distinguish between respiratory tract infections that require treatment and those that are self-limiting as well as several other diagnostic tools that can help clinicians identify pathogens at the point of care and define an appropriate treatment strategy earlier.
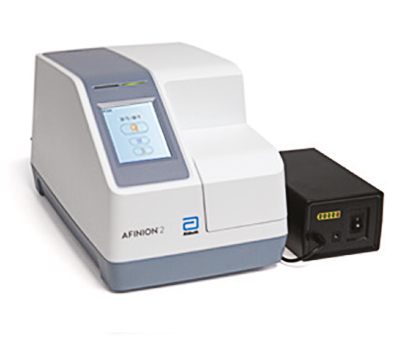
Afinion™ 2
The Afinion™ 2 analyzer is a compact, rapid, multi-assay analyser that provides valuable near patient testing at the point-of-care. With the Afinion System there’s no need to send test results to the lab or spend time tracking them down. That way you can keep your focus where it belongs – on the patient.

AFINION™ CRP
Afinion™ CRP is a rapid in vitro diagnostic test for quantitative determination of C-reactive protein (CRP) in human blood. In a recent evaluation of four CRP POC test, Afinion™ CRP achieved the best agreement with the central laboratory method and was judged to be the most user-friendly device.25
References
- EU Action on Antimicrobial Resistance. https://health.ec.europa.eu/antimicrobial-resistance/eu-action-antimicrobial-resistance_en
- The Lancet. Antimicrobial resistance: an agenda for all. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)01076-6/fulltext
- O’Neill J. Tackling drug-resistant infections globally: Final report and recommendations. Review on antimicrobial resistance 2016; https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf
- European Commission: Directorate-General for Health and Food Safety, Tackling antimicrobial resistance in a one health approach, Publications Office of the European Union, 2023; https://data.europa.eu/doi/10.2875/113990
- Shrestha P, Cooper BS, Coast J, Oppong R, Thuy N, Phodha T, et al. Enumerating the economic cost of antimicrobial resistance per‑antibiotic consumed to inform the evaluation of interventions affecting their use. Antimicrob Resist Infect Control 2018;7:98; https://doi.org/10.1186/s13756-018-0384-3
- OECD (2023), Embracing a One Health Framework to Fight Antimicrobial Resistance. OECD Health Policy Studies, OECD Publishing, Paris; https://doi.org/10.1787/ce44c755-en
- OECD. Stemming the Superbug Tide: Just A Few Dollars More. Paris: OECD Health Policy Studies, OECD Publishing (2018); https://www.oecd.org/en/publications/stemming-the-superbug-tide_9789264307599-en.html
- United Nations (2020). Global indicator framework for the Sustainable Development Goals and targets of the 2030 Agenda for Sustainable Development; https://unstats.un.org/sdgs/indicators/Global%20Indicator%20Framework%20a
- WHO: Antimicrobial resistance: Key facts. 21. Nov. 2023; accessed 07. Febr. 2025; https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- ECDC. Antimicrobial consumption in the EU/EEA (ESAC-Net) Annual Epidemiological Report for 2023; https://www.ecdc.europa.eu/en/publications-data/antimicrobial-consumption-eueea-esac-net-annual-epidemiological-report-2023. Accessed 07. Feb. 2025
- Smedemark SA, Aabenhus R, Llor C, Fournaise A, Olsen O, Jørgensen KJ. Biomarkers as point-of-care tests to guide prescription of antibiotics in people with acute respiratory infections in primary care. Cochrane Database Syst Rev 2022;10(10):CD010130; https://doi.org/10.1002/14651858.CD010130.pub3
- Cooke J, Llor C, Hopstaken R, Dryden M, Butler C. Respiratory tract infections (RTIs) in primary care: narrative review of C reactive protein (CRP) point-of-care testing (POCT) and antibacterial use in patients who present with symptoms of RTI. BMJ Open Resp Res 2020;7:e000624; https://doi.org/10.1136/bmjresp-2020-000624
- Van der Velden AW, van de Pol AC, Bongard E, Cianci D, Aabenhus R. et al. Point-of-care testing, antibiotic prescribing, and prescribing confidence for respiratory tract infections in primary care: a prospective audit in 18 European countries. BJGP Open 2022 ; 30;6(2); https://doi.org/10.3399/BJGPO.2021.0212
- GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet 2024; 404: 1199–226; https://doi.org/10.1016/S0140-6736(24)01867-1
- World Health Organization. (2022). Global antimicrobial resistance and use surveillance system (GLASS) report. https://iris.who.int/bitstream/handle/10665/364996/9789240062702-eng.pdf
- Llor C, Plate A, Bjerrum L, Gentile I, Melbye H, Staiano A, van Hecke O, Verbakel JY, Hopstaken R. C-reactive protein point-of-Care testing in primary care - broader implementation needed to combat antimicrobial resistance. Front. Public Health 2024;12:1397096; https://doi.org/10.3389/fpubh.2024.1397096
- ENASPOC – the European Network for Antibiotic Stewardship at the Point-of-Care. Accessed February 2025. https://www.enaspoc.com/
- Van Hecke O, Bjerrum L, Llor C, Melbye H, Hopstaken R, Gentile I, Plate A, Verbakel JY, Staiano A. Guidance on C-reactive protein point-of-care testing and complementary strategies to improve antibiotic prescribing for adults with lower respiratory tract infections in primary care. Front. Med., 2023. https://doi.org/10.3389/fmed.2023.1166742
- Staiano, A., Bjerrum, L., Llor, C., Melbye, H., Hopstaken, R., Gentile, I.I, Plate, A., van Hecke, O., & Verbakel, J. Y. (2023). C-reactive protein point-of-care testing and complementary strategies to improve antibiotic stewardship in children with acute respiratory infections in primary care. Frontiers in Pediatrics, 2023; https://doi.org/10.3389/fped.2023.1221007
- Anderson, M., Panteli, D., & Mossialos, E. (2024). Strengthening the EU response to prevention and control of Antimicrobial Resistance (AMR): Policy priorities for effective implementation. Copenhagen: WHO Regional Office for Europe. Licence: CC BY-NC-SA 3.0 IGO. ISBN: 1997-8073; https://eurohealthobservatory.who.int/publications/i/strengthening-the-eu-response-to-prevention-and-control-of-antimicrobial-resistance-(amr)-policy-priorities-for-effective-implementation
- Clerc, O., & Greub, G. (2010). Routine use of point-of-care tests: usefulness and application in clinical microbiology. Clinical Microbiology and Infection, 16(8), 1054-1061; https://doi.org/10.1111/j.1469-0691.2010.03281.x
- Gourlay A, Sutherland C, Radley A. Point-of-Care testing of HbA1c levels in community settings for people with established diabetes or people at risk of developing diabetes: A systematic review and meta-analysis. BMJ Open 2023;13(5):e072882; http://dx.doi.org/10.1136/bmjopen-2023-072882)
- Wubishet BL, Merlo G, Ghahreman-Falconer N, Hall L, Comans T. Economic evaluation of antimicrobial stewardship in primary care: a systematic review and quality assessment. J Antimicrob Chemother. (2022) 77:2373–88; https://doi.org/10.1093/jac/dkac185
- Tolley A, Bansal A, Murerwa R, Dicks JH. Cost-effectiveness of point-of-care diagnostics for AMR: a systematic review. J Antimicrob Chemother 2024; 79: 1248–1269; https://doi.org/10.1093/jac/dkae067
- Van Hoovels L, Massa B, Stavelin A, De Meyer H, De Schrijver P, Van Laethem V, Barglazan D, Gruson D, Hopstaken R, Peeters B, Van Hoof V, Verdonck A, Verbakel JY. Analytical performance and user-friendliness of four commercially available point-of-care devices for C-reactive protein. Clinica Chimica Acta 2024;560:119737; https://doi.org/10.1016/j.cca.2024.119737





