Global Point Of Care


Knowing your A1c IS THE FIRST STEP TO MANAGING IT
Welcome! This page is designed to help you understand the results of your HbA1c (or A1c) test and how to lower your A1c levels if they are high. Knowing your A1c is the first step in lowering your blood sugar to help manage your diabetes or prevent diabetes from developing in the first place.
Your A1c test was completed on the Afinion™ 2 Analyzer, which provides highly accurate results at your chosen point of care. The accuracy of Afinion 2 results have been clinically shown to match or even outperform routine laboratory methods.1,2
Now that you know your A1c results, find out what they mean and how you can improve them.
WHAT IS THE A1c TEST?
The A1c test is a simple, fingerstick blood test used to identify people with prediabetes and diagnose those with diabetes. It’s also used to monitor how well diabetes treatment is working over time. The test results provide you with a picture of your average blood glucose (blood sugar) level over the past 2 to 3 months. The higher your A1c levels, the greater your risk of developing diabetes and other problems.

THE ABCs OF DIABETES
A1c testing is part of the ABCs of diabetes—important steps you can take to prevent or delay future health complications.
A: Get a regular A1c test.
B: Try to keep your Blood pressure below 130/80 mmHg (or a target set by your doctor).
C: Manage your Cholesterol levels.
s: Stop Smoking or don’t start.
WHAT DO MY A1c NUMBERS MEAN?
Ideal A1c levels are different for everyone and can vary by age and other risk factors.
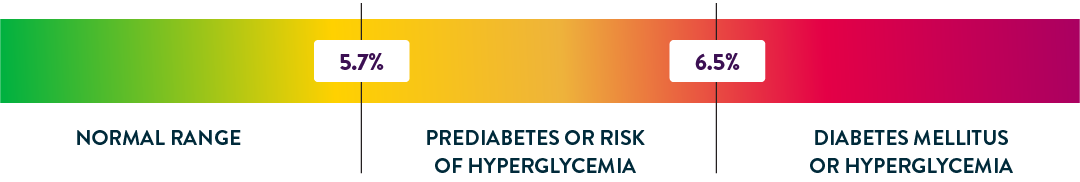
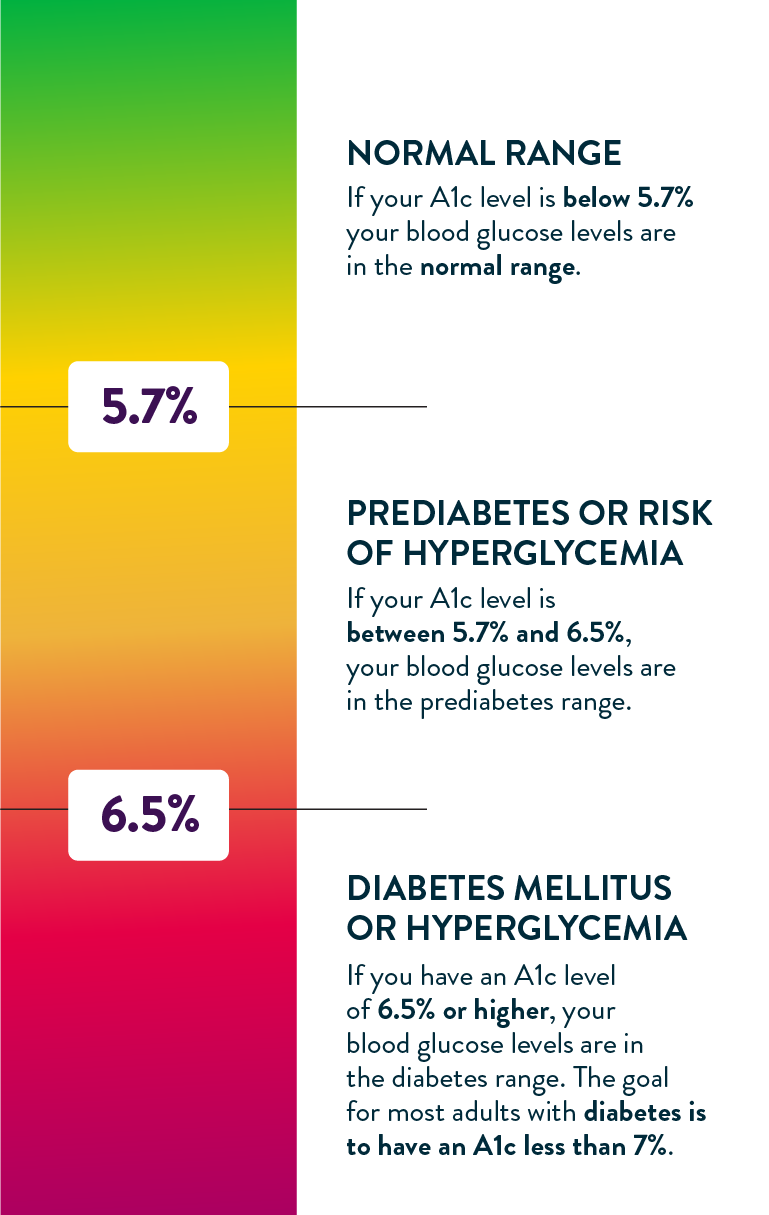
If your A1c level is below 5.7% your blood glucose levels are in the normal range.
If your A1c level is between 5.7% and 6.5%, your blood glucose levels are in the prediabetes range.
If you have an A1c level of 6.5% or higher , your blood glucose levels are in the diabetes range. The goal for most adults with diabetes is to have an A1c less than 7%.
What is Diabetes?
Categorized as type 1 or type 2, diabetes is a chronic disease that can increase your risk for serious health problems such as:
- Cardiovascular disease
- Chronic kidney disease
- Neuropathy (nerve pain)
- Hearing loss
- Stroke
- Osteoporosis and hip fractures
- Complications of the feet, eyes, mouth, and skin
People with type 1 diabetes do not produce insulin naturally. This requires monitoring A1c (average blood glucose levels) quarterly and glucose changes throughout the day, along with multiple daily injections of insulin with a pen or syringe, or the use of a pump. Insulin helps glucose from food get into cells so it can be used for energy.3
People with type 2 diabetes do not produce enough insulin, utilize it well, or both, so their cells can’t use blood glucose for the energy their bodies need. Medication and lifestyle changes can help manage type 2 diabetes.
What is prediabetes?
If you are diagnosed with prediabetes (5.7% - 6.4%), your blood glucose levels are above normal, but below diabetes levels. There are no clear symptoms of prediabetes, so you may not know you have it. And, although prediabetes can later develop into type 2 diabetes, it doesn’t have to be that way.
DIABETES PREVENTION: HOW TO LOWER YOUR A1c NATURALLY
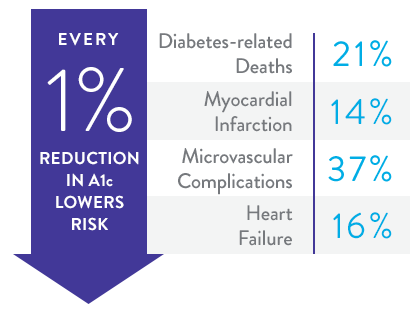
Making small changes to your lifestyle can help prevent or delay diabetes by reducing your A1c. And, if you already have diabetes, even small reductions in your A1c can reduce diabetes complications significantly.4
Your doctor will help you create a plan and set goals that work for you. They may also refer you to a Centers for Disease Control and Prevention (CDC) recognized, evidence-based lifestyle change program, like the National Diabetes Prevention Program or National DPP.
Consider these lifestyle changes to help lower your A1c naturally:
Lose weight
Being overweight raises your risk for type 2 diabetes, heart disease, high blood pressure, and stroke. Losing weight may help you prevent and manage these conditions—even losing 10-15 pounds can make a big difference. Here are some useful tips to help you lose weight for good.
Eat right
Good nutrition goes hand in hand with weight control, as well as diabetes prevention and management. All foods affect your blood glucose levels, but some will help you lower your A1c, while others will increase it. Check out these healthier eating suggestions.
Exercise regularly
Along with diet and medications, physical activity is important to preventing or managing diabetes. You don’t have to do strenuous exercise; you just need to be consistent and enjoy what you’re doing. See how to get started and inspired here.
Always consult with your physician/healthcare provider before making any dietary changes or beginning any exercise or weight loss program.
Frequently Asked Questions
HOW OFTEN SHOULD I CHECK MY A1c?
Your doctor will tell you how often you need the A1c test, but usually you’ll have the test at least twice a year if you’re meeting your treatment goals. If you're not meeting your goals or you change treatments, you may need to get an A1c test more often.
A general guideline for A1c testing is:
Every 6 months if your last A1c was in goal range
Every 3 months if your medications have changed or your last A1c was not in goal range
WHAT IS eAG AND HOW IS IT DIFFERENT FROM A1c?
Your doctor may report your A1c results as eAG or “average glucose.” Your eAG reading directly correlates to your A1c value, but it is reported in mg/dL (milligrams per deciliter), the same unit of measurement shown on blood glucose meters and continuous glucose monitors (CGMs) used at home.
The catch is that eAG/A1c is not the same average glucose level as the average of the readings on your meter. Monitoring measures your blood glucose at a moment in time, whereas eAG/A1c represents an average of your glucose levels 24 hours a day, including times when people are less likely to check their blood sugar (for example, post-meal periods of higher blood sugar).
The American Diabetes Association suggests an A1c of 7 percent for nonpregnant adults, which is an eAG of 154 mg/dL, but more or less stringent glycemic goals may be appropriate for each individual. To convert your eAG reading to A1c and vice versa, use this calculator.
WHAT ARE THE SYMPTOMS OF DIABETES?
The following symptoms of diabetes are typical, however, some symptoms are so mild that they may go unnoticed. Early detection and treatment of diabetes can decrease the risk of developing complications.
- Frequent urination
- Feeling very thirsty
- Feeling very hungry even though you are eating
- Extreme fatigue
- Blurry vision
- Cuts and bruises that are slow to heal
- Weight loss even though you are eating more
- Tingling, pain, or numbness in the hands or feet
WHAT IS GESTATIONAL DIABETES?
Gestational diabetes occurs in up to 10 percent of pregnancies in the US every year. It is not known what causes it, but we do know that women who develop it can still have a healthy baby. We also know that women who acquire it did not necessarily have diabetes before becoming pregnant, nor will they necessarily continue to have it after giving birth. However, acting quickly after diagnosis is very important for the health of the mother and baby. Beginning treatment early is crucial to combatting gestational diabetes.
HOW DO CARBOHYDRATES AFFECT MY BLOOD GLUCOSE?
When you consume food or beverages with carbohydrates (carbs) your body breaks them down into sugar (glucose), raising glucose levels in your blood. In people without diabetes, the pancreas releases insulin to help your cells absorb the excess glucose. When blood sugar goes too high, it’s known as hyperglycemia. When blood sugar drops too low, it’s known as hypoglycemia.
Both hyperglycemia and hypoglycemia can be dangerous if they aren’t treated promptly, resulting in potentially life-threatening conditions, so it’s important to act quickly to restore blood sugar to normal levels.
WHICH CARBOHYDRATES SHOULD I EAT AND WHICH SHOULD I AVOID?
If you have diabetes or prediabetes and are trying to lower your A1c, the best foods to eat are whole, unprocessed, non-starchy vegetables. These mostly green, leafy vegetables have few carbohydrates, so they have the least impact on your blood sugar.
- Lettuce
- Cucumbers
- Broccoli
- Tomatoes
- Green beans
Healthy foods that contain starchy carbohydrates are fine to eat as well, but in smaller quantities. These include fruits, intact whole grains, and some starchy vegetables like:
- Apples
- Berries
- Cantaloupe
- Brown rice
- Whole wheat bread
- Oatmeal
- Corn
- Sweet potatoes
Foods to avoid eating include refined, highly processed carbohydrates and foods with added sugar, including:
- Soda
- Sweet tea
- Fruit juice
- White bread
- White rice
- Sugary cereal
- Sweets and candy
- Chips
This web page references information from the American Diabetes Association website: https://diabetes.org/ and the Centers for Disease Control and Prevention website: https://www.cdc.gov/.
REFERENCES: 1. NGSP. Harmonizing Hemoglobin A1c Testing. http://ngsp.org/ Accessed May 1, 2024. 2. The EurA1c Trial Group. EurA1c: The European HbA1c Trial to Investigate the Performance of HbA1c Assays in 2166 Laboratories across 17 Countries and 24 Manufacturers by Use of the IFCC Model for Quality Targets. Clin Chem. 2018;64(8):1183-1192. http://clinchem.aaccjnls.org/content/clinchem/64/8/1183.full.pdf. 3. American Diabetes Association, Understanding A1c. https://www.idf.org/aboutdiabetes/what-is-diabetes.html. Accessed May 1, 2024. 4. Stratton IM, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective Observational Study. BMJ. 2000;321(7258):405-412. doi:10.1136/bmj.321.7258.405


