Global Point of Care
are you a point-of-careologist?



Point-of-care testing: quick results for quick decision-making
In the early 1970s, medical scientist and bioengineer Dr Gerald Kost conceptualized a new field of patient-focused testing. Performing biosensor-based measurements of ionized calcium in whole blood at the bedsides of patients receiving liver transplants, he facilitated the reporting of immediate results and improved patient outcomes.1 By the 1980s, he validated the self-named “point-of-care” testing, by performing whole-blood analysis in operating rooms at the patient’s side.1
Since then, point-of-care tests (POCTs) have proliferated due to advances in molecular biology and the pressing need for rapid results. Today, POCT has given rise to a new medical field called “Point-of-Careology.”1 Here are a few reasons to consider becoming a Point-of-Careologist, especially if you are interested in diabetes or cardiovascular disease management.
Compliance With HbA1c POCTs
Studies have shown that POCTs improve patient compliance and outcomes. One study looked at patient satisfaction with POCT hemoglobin A1c.2 Before and after POCT implementation, patient adherence to doctors’ recommendations for testing frequency increased from 24 to 85%.2 Additionally, patient satisfaction was high.2 Mean HbA1c levels across 75 patients significantly improved for better glycemic control.2 Another recent study concluded that the use of HbA1c POCT led to an improved practice workflow and increased the satisfaction of physicians, staff and patients.3 The number of required patient visits was reduced by 80% and the number of venous blood collections was reduced by 75%.3 Eighty-two percent of patients were able to discuss their HbA1c values with physicians during their first visit.3 Early consultations promote early interventions and better compliance.
POCTs Improve Costs, Safety, Access to Care
In the urgent care setting, the usefulness of POCTs was validated in combination with a written staff protocol for diabetes screening for the asymptomatic population.5 The results of a questionnaire given during the study are shown below.
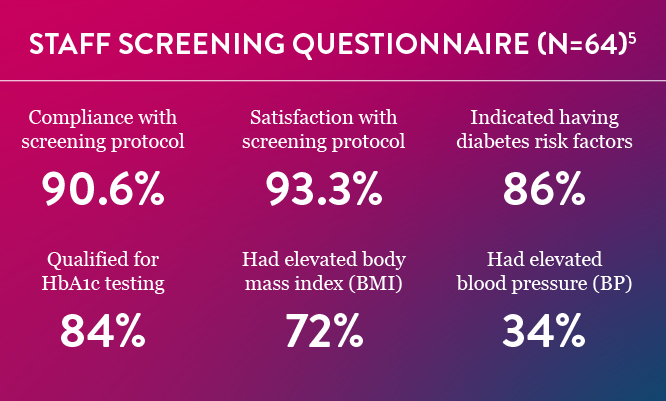
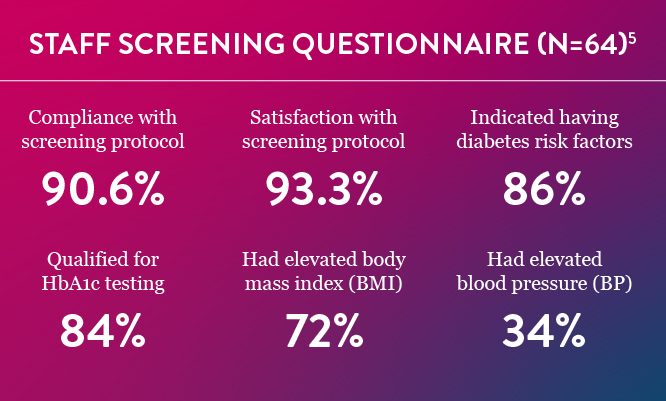
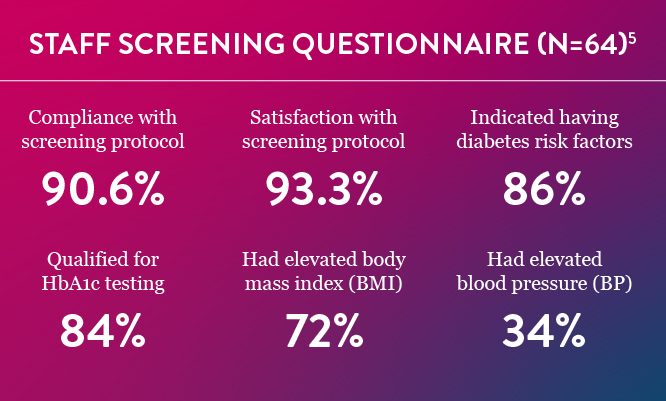
Data from the study demonstrated that almost 16% of the participants had previously undiagnosed, asymptomatic prediabetes or diabetes.5 Earlier diagnosis and treatment would lead to fewer complications, lower costs for patients, and reduce visits to an Emergency Department, which causes a significant financial burden to the health care system as a whole.5
Brazilian researchers found that POCT HbA1c devices used in primary care units improved the access to A1C tests and increased the rate of early control of blood glucose. During a 10-year period, the POCT group had similar costs but higher effectiveness when compared to the control group using laboratory testing. In rural and undeveloped areas, POCTs were recommended to improve patient outcomes by a consortium of noted health care professionals.4 They asserted that, in resource-limited areas with no centralized lab, POCTs may help reduce health care disparities.4
Implementation of POCT at an ambulatory practice at an academic medical center significantly improved clinical operations by reducing costs through better efficiencies.6 They noted a 21% decrease in tests ordered per patient, an 89% decrease in follow-up phone calls, and a 61% reduction in patient revisits.6 They estimated potential costs savings from these improved efficiencies at approximately $25 per patient.6
Modern Challenges Met by POCTs
A recent US government report found that Medicare telehealth use increased 63-fold from 2019 to 2020.7 Since the arrival of COVID-19 and the shift to working from home, more and more consumers are demanding telemedicine, fewer on-site clinic visits, rapid tests and diagnoses—propelling the need for POCTs. Due to fewer patient revisits, POCTs have the potential to reduce viral exposure for both patients and medical staff. POCTs connected to an internet device can transmit data ahead of a patient’s admission by ambulance or during transfer between facilities. When POCTs are integrated with electronic medical records, results can be shared for a multidisciplinary approach to patient care and follow-up treatments. POC testing has become more automated which further reduces errors and operator time while enhancing safety and quality.
POCTs are convenient tools to assist in timely patient diagnoses, improve access to care, and strengthen patient compliance and satisfaction. By becoming a Point-of-Careologist, you will help meet these modern challenges by placing the emphasis on care and reducing emphasis on waiting for lab results.
References
- Liu X, Zhu X, Kost G, et al. The creation of point-of-careology. Point of Care. 2019;18: 77-84.
- Al Hayek AA, Al-Saeed AH, Alzahrani WM, Al Dawish MA. Assessment of patient satisfaction with on-site point-of-care hemoglobin A1c testing: An observational study. Diabetes Ther. 2021;12(9):2531-2544. doi:10.1007/s13300-021-01126-7
- Patzer KH, Ardjomand P, Göhring K, et al. Implementation of HbA1c point of care testing in 3 German medical practices: Impact on workflow and physician, staff, and patient satisfaction. J Diabetes Sci Technol. 2018;12(3):687-694. doi:10.1177/1932296818759690
- Drain PK, Hyle EP, Noubary F, et al. Diagnostic point-of-care tests in resource-limited settings. Lancet Infect Dis. 2014;14(3):239-249. doi:10.1016/S1473-3099(13)70250-0
- Clark SR, Wilson, ML. Original research: Early diabetes screening in the urgent care, Part 2. JUCM. (2022) https://www.jucm.com/original-research-early-diabetes-screening-urgent-care-part-2/
- Crocker JB, Lee-Lewandrowski E, Lewandrowski N, Baron J, Gregory K, Lewandrowski K. Implementation of point-of-care testing in an ambulatory practice of an academic medical center. Am J Clin Pathol. 2014;142(5):640-646. doi:10.1309/AJCPYK1KV2KBCDDL
- Madjid K, Lee EC, et al. National survey trends in telehealth use in 2021: Disparities in utilization and audio vs video services, ASPE Issue Brief. (2022) https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf