Global Point of Care
Diabetes and HbA1c:
Facts and Stats



CHRONIC DISEASE VISIT STATISTICS
When clinicians contemplate their daily patient load in the primary care setting, most of it is comprised of chronic diseases. According to CDC data published in 2016, thirty-seven percent (37%) of patient visits involve a pre-existing chronic disease state. While an additional 27% accounts for “new problems”, which may ultimately turn out to be a first visit for a chronic illness.1-6
In 2016, there were over 883.7 million primary care visits. It’s estimated that over 326 million of these were chronic care visits.1-6 In this context, age matters. The number of people over 65 visiting physicians for chronic conditions was 51%.1-6 According to the CDC, over 63% of patients over 65 have at least 2 comorbidities.2-7 As the US population continues to age, two things are certain;
- the number of patients with chronic conditions will continue to rise and
- the number of comorbidities these patients experience increases with age.
Diabetes Incidence
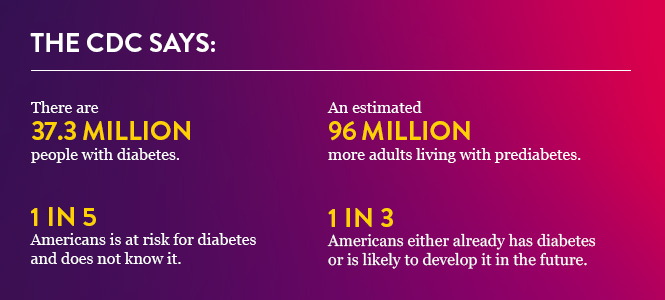
So, there is a high probability that every primary caregiver examines people with diabetes every day.
More likely than not, patients that present to the physician have type 2 diabetes, not type 1. The CDC estimates that more than 90% of people with diabetes in the US, diagnosed or otherwise, have type 2 diabetes.3 And since most people with type 2 diabetes have their onset in adulthood, it is likely that many of them are currently undiagnosed.
It is also likely that practicing clinicians are examining patients who should be screened for diabetes and its complications. Therefore, nearly every clinician experiences the need to diagnose and treat diabetes daily and while they may not be intimately familiar with the statistics, they see diabetes and its complications frequently.
Diabetes Morbidity
In addition to its increasing incidence, diabetes is also one of the most serious chronic conditions encountered by clinicians daily. The rise in diabetes incidence runs counter to trends with most of the rest of the leading causes of morbidity and mortality. While most of the leading causes of morbidity and mortality have been declining from the middle of the last century until the advent of the COVID-19 pandemic, diabetes persistently resists declining.
Currently, diabetes incidence is increasing by 14.8%, the highest increase of any of the leading causes of death.2 Diabetes may be an underlying disease state that is associated with more comorbidities than any other.4
Where does all this data lead us? It provides some inescapable conclusions, including that diagnosis of type 2 diabetes needs to be a focus in every American primary care practice.
While diabetes incidence is related to income level and socioeconomic status, there is no group that is immune.5 Engaging in exercise and healthy eating habits is the right patient approach to reduce the likelihood of developing type 2 diabetes, but with the extraordinarily large group of undiagnosed prediabetic patients, effective screening programs across primary care is vital in reducing morbidity, mortality and related costs.
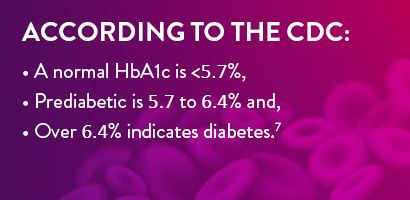
Effective diabetes screening leads to improved quality of life when early diagnosis reduces the onset of diabetes-related health complications. By far, HbA1c is the preferred method to diagnose prediabetes and follow up on progress with patients presenting as either prediabetic or who have been diagnosed as diabetic.6
Diabetes Management
In the past, diabetes management was largely a matter of advising people with diabetes to avoid carbohydrates, test their glucose levels frequently and engage in at least a modest amount of exercise. To a large extent, people with diabetes did not follow these recommendations by actually making a significant change in their life style and eating habits.
In recent years, more effective medications have become available to treat type 2 diabetes. These new management tools include continuous glucose monitoring for people with type 1 diabetes and novel new diabetic medications including semaglutide and other biosimilars for people with type 2 diabetes. As a result, treatment of people with type 2 diabetes has improved from the days of “watch your diet, get some exercise and come back and see me in three months”.
Once a person with type 2 diabetes has been diagnosed, novel treatment options involve improving control, lowering HbA1c, and improving clinical outcomes.
The prognosis for the newly diagnosed person with diabetes is better than before and can help them to take responsibility for making life changes that, in combination with effective diagnosis and treatment programs, give them the prospect of a longer, healthier life.
References
- Products - Data Briefs - Number 331 - January 2019 (cdc.gov) CDC review of patient care statistics
- Prevalence of Multiple Chronic Conditions Among US Adults, 2018 (cdc.gov) CDC comorbidity by age data
- By the Numbers: Diabetes in America | Diabetes | CDC: Incidence of diabetes and pre-diabetes in the US
- FastStats - Leading Causes of Death (cdc.gov): CDC report on the leading causes of death in the US
- 12 Diabetes Data and Statistics | CDC
- Consensus Statement on the Worldwide Standardization of the Hemoglobin A1C Measurement | Diabetes Care | American Diabetes Association (diabetesjournals.org): ADA proof source on utility of A1C for diagnosis and monitoring of diabetes
- Diagnosis and treatment - Mayo Clinic: discussion by Mayo Clinic of A1C testing