Global Point of Care
The role of ACR Testing in Value-Based Care (VBC)

Kidney disease affects 37 million American adults, but 90% are unaware they even have it1. The goal is to change that dynamic with HEDIS and MIPS quality measures tied to ACR testing.
It’s been known that HbA1c is a key quality measure for HEDIS, but the addition of urine ACR or eGFR testing to HEDIS is designed to improve chronic kidney disease (CKD) testing in people with diabetes1. People with diabetes have the highest risk of CKD and are the most expensive members in the healthcare system. The goal is to improve health metrics by more consistently identifying and treating chronic kidney disease in this high-risk population2.
Chronic kidney disease, which can be identified with ACR testing, occurs in 20-40%3 of all people with diabetes and these patients are at 1.9 times higher risk of needing dialysis4. While early achievement of HbA1c results to target goals is associated with lowering risk of microvascular complications5, left undetected, CKD gets worse over time and can lead to major comorbidities1,4. Which is why, the National Kidney Foundation recommends an annual kidney health evaluation for people with diabetes, with eGFR and urine ACR testing, to identify and mitigate risk to progression1,2,6,7. And yet, while ACR testing is widely available and inexpensive, less than 50% of people with diabetes actually receive annual ACR testing1. Point-of-care solutions can help enhance reach and accessibility to testing, conveniently, at the site of care.
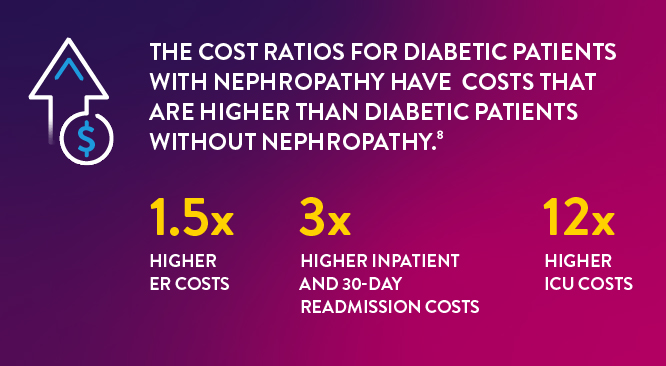
Financial impact of Diabetes & Nephropathy to the Healthcare Institution:
Diabetic patients with nephropathy leads to higher costs for healthcare institutions with higher readmission and ICU visits and even far greater overall costs to institutions for advanced diabetic patients. The cost ratios for diabetic patients with nephropathy have ER costs that are 1.5-times higher, inpatient and 30-day readmission costs that are 3-times higher and ICU costs 12-times higher than diabetic patients without nephropathy.8
Identifying diabetic patient risk of or progression to chronic kidney disease with ACR testing can be the first step to driving improved outcomes and cost-effective care for this patient group. In a 2022 screening study of individuals at high risk of chronic kidney disease*, point-of-care testing identified 20.4% of people – people who previously were unaware of their condition, were identified – simply by screening using a POC ACR Test.9 The majority (96%) of patients in this study felt POCT was convenient and that immediate results and feedback helped them better understand their condition.9
Identifying diabetic patient risk of or progression to chronic kidney disease with ACR testing can be the first step to driving improved outcomes and cost-effective care.
The role of POC ACR testing in the Value-Based Care Model better enables patients and providers to immediately screen and monitor diabetic patients throughout their disease course to decrease patient morbidity and curb the increasingly elevated costs tied to these high-risk patients.
Improvement in Care with HbA1c and ACR testing leads to lower costs:
Clinically, every 1% reduction in HbA1c levels leads to 37% reduction in microvascular complications5; including nephropathy and dialysis. Financially, reductions in HbA1c leads to a 1% reduction in HbA1c a 2% reduction in all cause total costs and a 13% reduction in diabetes-related costs10. Complementing HbA1c testing with annual ACR testing, will help to identify and treat chronic kidney disease more effectively. Enhancing earlier identification of this diabetes-related morbidity and cost can lead to improved quality rates and enhance more cost effective care over time.
POC testing can help improve testing for patients with diabetes and can help patients by immediately identifying patients at risk of chronic kidney disease. Results in minutes at the site of care enables immediate patient-provider consultation for best patient management and outcomes. More importantly getting tested can be a proactive contributor to improving health outcomes which may ultimately lead to improvements in health metrics and more cost-effective care for patients using value based care model as its designed to encourage.
*High risk are individuals with a previous diagnosis of diabetes or hypertension, age over 50 years, first-degree relatives with end-stage kidney disease.
References
- Chronic Kidney Disease in the United States, 2021. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021. https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html
- National Kidney Foundation. Kidney Health Evaluation Measure. Accessed April 27, 2023. https://www.kidney.org/content/kidney-health-evaluation-measure
- National Committee for Quality Assurance. Kidney Health Evaluation for Patients with Diabetes (KED). Accessed April 27, 2023. https://www.ncqa.org/hedis/measures/kidney-health-evaluation-for-patients-with-diabetes/
- Gabby RA et al., Clinical Diabetes 2020; 38 (4) :371-381
- Definitive Healthcare, US HbA1c Claims Medical Clearing House; May-June 2022.
- Stratton I et al., Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study; www.ncbi.nlm.nih.gov/pmc/articles/PMC27454/.
- Brock M, NCQA. Kidney Health: A New HEDIS Measure. Accessed April 27, 2023. https://www.ncqa.org/blog/kidneyhealth.
- 8. NCQA. Kidney Health Evaluation for Patients with Diabetes (KED). Accessed April 27, 2023. https://www.ncqa.org/hedis/measures/kidney-health-evaluation-for-patients-with-diabetes/
- Definitive Healthcare, US HbA1c Claims Medical Clearing House; August – October 2022.
- Vassalotti JA and Boucree SC. Integrating CKD Into US Primary Care: Bridging the Knowledge and Implementation Gaps. Kidney Int Rep. 2022 Feb 4;7(3):389-396. doi: 0.1016/j.ekir.2022.01.1066. PMID: 35257053; PMCID: PMC8897496.
- Lage MJ and Boye KS, Current Medical Research and Opinion 2020; 36(9):1441-1447. 10.1080/03007995.2020.1787971. https://doi.org/10.1080/03007995.2020.1787971