Global Point of Care
Point of Care Highlights
Featured Products
i-STAT 1 Wireless
Learn how the i-STAT 1 Wireless provides the ability to perform diagnostic tests and upload results to your EMR automatically from many patient-care areas.
i-STAT CHEM8+ Cartridge
With i-STAT CHEM8+, healthcare professionals can obtain chemistries, electrolytes, hematocrit and hemoglobin levels in approximately two minutes without leaving the patient's side.
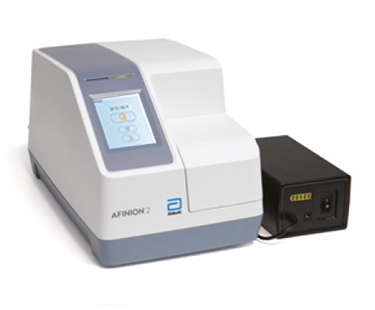
AFINION™ 2
The Afinion™ 2 analyzer is a compact, rapid, multi-assay analyzer that provides valuable near patient testing at the point-of-care. With the Afinion™ System, there’s no need to send test results to the lab or spend time tracking them down.
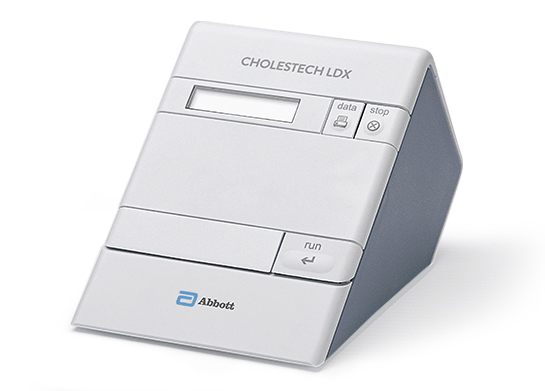
CHOLESTECH LDX™ ANALYZER
The Cholestech LDX™ Analyzer empowers healthcare professionals and patients with a lab-accurate complete lipid profile and glucose in 5 minutes per test cassette.
Service. Support. Answers.
Get all the detailed technical support and service you need – the way you need it. We’re here for you online and over the phone.


Service. Support. Answers.
Get all the detailed technical support and service you need – the way you need it. We’re here for you online and over the phone.